Trying to understand BPD vs. Bipolar? You’re in the right place. Both disorders can seem similar but have crucial differences in symptoms, causes, and treatments. This article will help you clearly distinguish between Borderline Personality Disorder and Bipolar Disorder.
Key Takeaways
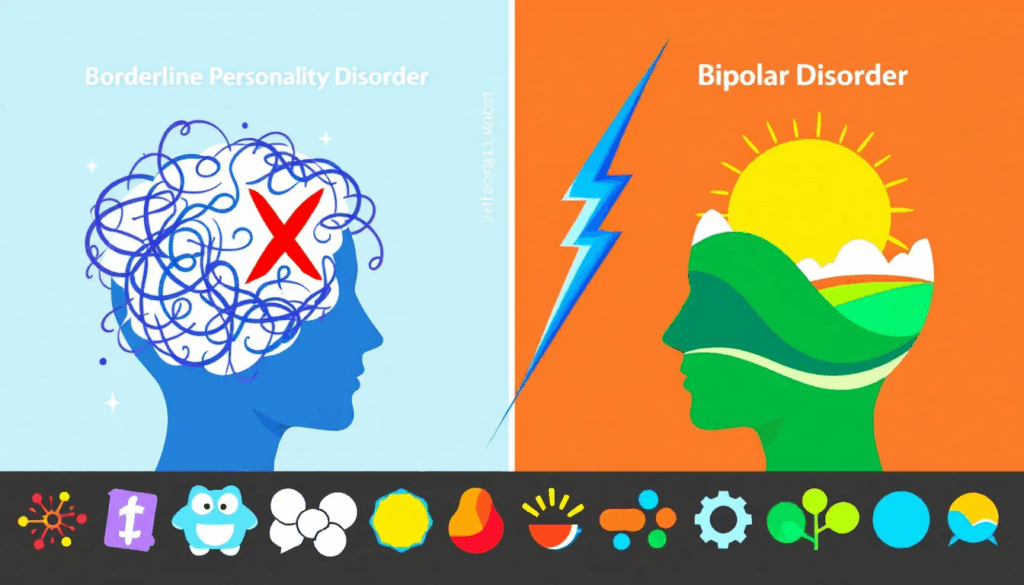
Borderline Personality Disorder (BPD) is a personality disorder characterized by extreme emotional instability and chaotic relationships, while bipolar disorder is a mood disorder marked by prolonged manic and depressive episodes.
Diagnosis and treatment differentiate BPD and bipolar disorder, with BPD requiring five of nine specific symptoms for diagnosis, while bipolar disorder relies on mood history and physical exams; accurate diagnosis is critical for effective management.
Co-occurrence of BPD and bipolar disorder increases the complexity of treatment, elevating risks for suicidal behavior and substance use disorders, necessitating comprehensive assessments for proper care.
Understanding Borderline Personality Disorder (BPD) and Bipolar Disorder
Borderline personality disorder (BPD) and bipolar disorder are distinct types of mental health disorders, with BPD falling under the umbrella of personality disorders—more precisely, Cluster B personality disorders known for intense and unpredictable behavior patterns. Bipolar disorder, on the other hand, is classified as a mood disorder that causes individuals to experience profound shifts in mood ranging from manic highs to depressive lows. Though some symptoms may overlap between BPD and bipolar disorder—as well as other types of personality disorders—they represent separate medical diagnoses.
In the United States, approximately 1.4% of adults grapple with borderline personality disorder. Meanwhile, a considerable number also deal with the impact of bipolar disorder on their lives. Those afflicted by BPD typically struggle enduringly with heightened emotional responses, difficulty managing emotions effectively and maintain tumultuous relationships. These challenges tend to first emerge during early adulthood, but often lessen later in life around one’s mid-30s or 40s. While instances exist where younger adolescents show signs associated with BPD primarily emerges after adolescence.
The assessment process for both bipolar disorder and borderline personality can be intricate due to how profoundly an individual’s symptoms affect daily living—often resulting in a whirlwind existence characterized by extreme emotive states and experiences distinguishing them from each other holds significant importance when seeking appropriate treatment methodologies designed specifically for either condition.
Key Symptoms of BPD vs. Bipolar Disorder
Bipolar disorder and BPD (Borderline Personality Disorder) differ chiefly in the duration and causation of mood shifts. People with BPD often experience sudden changes in mood as a reaction to interpersonal issues, typically lasting mere hours. Conversely, bipolar disorder is marked by intense mood swings that can manifest as severe manic or depressive episodes enduring weeks or even months at a time. These conditions are complicated when other mood disorders come into play.
Although distinct, BPD and bipolar disorder exhibit similar symptoms which complicate their differentiation: irritability, attention difficulties, and swiftly changing thoughts are common to both conditions. Such overlapping features make daily life management challenging for those affected. Both illnesses can lead to impulsive actions, suicidal ideation, and fluctuating emotional states. Biploar involves defined cycles of highs (mania) or lows (depression), whereas BPD’s pervasive changes aren’t limited within such clear-cut boundaries but also present comparable traits complicating precise diagnosis.
Specific indicators unique to BDP encompass an intense fear of abandonment—whether it be actual or perceived—a tendency towards impulsiveness along with turbulent relationships and self-concept fluctuations where individuals may go great lengths evading abandonment scenarios they believe might occur. Recognizing these critical variances between each condition’s particular symptoms plays a pivotal role in ensuring an accurate diagnostic conclusion leading to proper treatment avenues.
Causes and Risk Factors
Both BPD and bipolar disorder originate from a complex interplay of genetic, environmental, and temperamental factors. Having psychiatric disorders within the family substantially increases the risk for both conditions, with those having a first-degree relative diagnosed with BPD being fivefold more susceptible to developing it themselves.
The environment one is exposed to during their early years can play an influential role in triggering these mental health issues. Harrowing experiences such as childhood abuse or emotional neglect are linked to an increased likelihood of experiencing both BPD and bipolar disorder later in life. Instances of familial discord and emotional distress throughout childhood may elevate the chances of someone developing bipolar disorder.
Certain personality characteristics like high levels of activity or instability in emotions might presage the manifestation of either condition. The onset of BPD has also been associated with persistent disruptions in sleep patterns. Especially noteworthy is that encountering emotional trauma during one’s youth bears specific relevance to predicting the future development of BPD. Being aware of these predisposing elements can be crucial for timely detection and proactive management efforts concerning these mental health challenges.
Diagnostic Criteria for BPD and Bipolar Disorder
The process of identifying BPD and bipolar disorder utilizes distinct benchmarks and methodologies. Diagnosing BPD typically occurs after an individual reaches the age of 18, given the developmental aspects of personality traits. This diagnosis hinges on long-term observation of behavioral patterns to determine functional capacity. Evaluating a patient’s behaviors and emotional state through a mental status examination is essential.
For a BPD diagnosis according to the DSM-5, patients must exhibit at least five out of nine designated symptoms such as an intense fear of abandonment, impulsiveness, or having unstable relationships. Although diagnostic criteria for bipolar disorder diverge clearly from those for BPD, similar signs can obscure the diagnostic pathway. The presence of shared symptoms underscores why it is critical that experienced professionals perform comprehensive evaluations.
Securing an accurate diagnosis enables individuals with these conditions to obtain care specifically catered to their unique mental health condition—key in managing treatment effectively. With commonality seen in overlapping manifestations among various mental illnesses, this accentuates just how vital meticulous assessments are within the realm of diagnosing mental health disorders.
The Impact on Relationships
Interpersonal relationships can be severely affected by both BPD and bipolar disorder. Those with BPD may experience a fluctuating self-image and engage in unstable relationships, which often leads to unpredictable interactions. The intense emotions linked with BPD might cause individuals to alternate between excessively admiring and sharply devaluing their partners, contributing to stormy connections filled with discord and occasional conflicts characterized by profound emotional intensity.
When dating someone who has BPD, the early stages may include periods of significant idealization that can abruptly switch to harsh criticism during moments of strife. People diagnosed with BPD tend to oscillate between extreme views of others as entirely virtuous or utterly flawed. Trust within these partnerships is frequently compromised due to impetuous behaviors like dishonesty.
Employing methods such as setting clear boundaries and advocating for professional therapy could foster greater stability in associations involving people suffering from BPD. Understanding underlying abandonment issues might assist partners in managing the complex emotional landscapes posed by those living with this condition. Providing education about the nuances of dealing successfully with someone diagnosed with borderline personality disorder also equips family members better support afflicted loved ones.
Co-occurrence of BPD and Bipolar Disorder
Individuals may receive a diagnosis that includes both borderline personality disorder and bipolar II disorder. Roughly 20% of individuals with bipolar II disorder and approximately 10% who have been diagnosed with type I bipolar are also found to suffer from comorbid borderline personality disorder (BPD). For those living with BPD, being Burdened by bipolar illness can result in more frequent hospital admissions and less favorable outcomes when undergoing treatment.
The likelihood of engaging in suicidal behaviors is notably increased for patients grappling with the dual diagnoses of borderline personality disorder and either form of bipolar condition compared to having just one such mental health issue. A heightened incidence of substance abuse disorders has been linked to cases where BPD occurs alongside bipolar disorder, often leading to longer durations within hospitals as well as escalated healthcare expenditures during their care regimen.
For the precise identification of co-occurring conditions like borderine personailty disorder among other mental health issues, proper assessments drawing upon diverse viewpoints are crucial. It’s estimated that nearly two-fifths of people suffering from BPD might erroneously be identified as having only bipolar rather than detecting concurrent conditions.A self-medicating tendency among those coping with biological problems frequently escalates into additional complications such as substance misuse or dependence on alcohol, which hampers effective treatment strategies.
Treatment Options for BPD and Bipolar Disorder
A variety of treatment methods are utilized for BPD and bipolar disorder, typically encompassing both therapeutic interventions and medication. Dialectical Behavior Therapy (DBT) has been tailored specifically to assist those with BPD in regulating their emotional responses. Participating in group therapy sessions and receiving family education may also play a significant role in effectively managing the symptoms associated with BPD.
For those dealing with BPD, psychotherapy stands as a cornerstone of treatment while Cognitive Behavioral Therapy (CBT) is useful for diminishing mood swings and anxiety among individuals grappling with bipolar disorder. Although there are no medications exclusively sanctioned for treating BPD, various drugs might be prescribed to mitigate symptoms present in both conditions. In regards to bipolar disorder, the dual approach of therapy combined with medication constitutes the primary mode of treatment. At times, hospitalization becomes imperative when patients exhibit acute symptoms related to either condition necessitating safeguarded observation and concentrated care.
Integrating lifestyle modifications such as consistent physical activity and maintaining a balanced diet can bolster effective management strategies for both disorders. Ensuring an accurate diagnosis remains paramount since it not only directs appropriate treatments but also enhances symptom control within individuals who manifest coexisting mental health issues.
Importance of Accurate Diagnosis
Ensuring that individuals with borderline personality disorder (BPD) or bipolar disorder receive the correct diagnosis is crucial for providing them with effective treatment, as it allows for care that is specifically suited to their unique needs. The process of diagnosing and treating BPD can be challenging due to many people being unaware they have this personality disorder.
To diagnose someone with borderline personality disorder, a presence of at least five out of nine established symptoms must be identified consistently across various situations over time. In contrast, bipolar disorder diagnoses rely on physical examinations and a detailed history of symptoms. For optimal symptom management and improved outcomes, it’s essential to keep lines of communication open with healthcare professionals.
Living with BPD and Bipolar Disorder
Managing BPD and bipolar disorder necessitates continuous attention and assistance from a mental health professional with appropriate qualifications. The mastery of symptom management for those living with bipolar disorder is crucial in the context of their treatment plan, including setting up consistent daily routines to foster better control over symptoms associated with both BPD and bipolar, thus enhancing stability.
For individuals grappling with BPD and bipolar disorder, implementing mindfulness practices can be instrumental in achieving emotional regulation. Incorporating regular exercise into one’s lifestyle can lead to an improvement in mood as well as a reduction in the symptoms prevalent across both conditions, thereby bolstering overall emotional well-being and leading to higher levels of positive emotionality. The journey toward managing emotions effectively along with controlling symptoms linked to BPD typically unfolds incrementally, demanding persistent dedication.
Summary
Understanding the key differences and treatment options for BPD and bipolar disorder is crucial. Both conditions have unique symptoms, causes, and diagnostic criteria that require careful evaluation by qualified professionals. Accurate diagnosis ensures that individuals receive the appropriate treatment tailored to their specific needs.
Living with BPD and bipolar disorder can be challenging, but with the right support and treatment, individuals can lead fulfilling lives. Whether through therapy, medication, or lifestyle changes, managing these conditions is possible. Remember, knowledge and understanding are the first steps toward effective treatment and improved mental health.
Frequently Asked Questions
Can a person have both BPD and bipolar disorder?
Yes, a person can be diagnosed with both borderline personality disorder and bipolar disorder, which can complicate treatment and elevate the risk of suicidal behavior and substance use disorders.
What are the main differences between BPD and bipolar disorder?
The main differences between BPD and bipolar disorder are the duration and triggers of mood changes; BPD features rapid mood shifts triggered by interpersonal stress, whereas bipolar disorder involves prolonged manic or depressive episodes lasting weeks or months.
How is BPD diagnosed?
BPD is diagnosed by observing behavioral patterns over time, needing at least five out of nine symptoms as outlined in the DSM-5 criteria.
This systematic approach ensures an accurate diagnosis of the disorder.
What treatment options are available for bipolar disorder?
Treatment options for bipolar disorder include Cognitive Behavioral Therapy (CBT), medication, lifestyle changes, and possibly hospitalization for severe symptoms.
These approaches aim to stabilize mood and improve overall functioning.
How can relationships be managed when one partner has BPD?
Managing a relationship with a partner who has BPD requires the establishment of healthy boundaries and a deep understanding of their fears of abandonment.
Encouraging professional treatment is also essential for stabilizing the relationship.
Author

Board-Certified Psychiatric Mental Health Nurse Practitioner with undergraduate degrees in Psychology and Philosophy (Summa Cum Laude) from Plymouth State University, and MSN degrees from Rivier and Herzing Universities. Specializing in PTSD, mood, anxiety, and personality disorders, with expertise in psychodynamic therapy, psychopharmacology, and addiction treatment. I emphasize medication as an adjunct to psychotherapy and lifestyle changes.