Bipolar disorder includes Bipolar 1 and Bipolar 2. The main difference is that Bipolar 1 involves full manic episodes, while Bipolar 2 involves hypomania and depression. In this article, we will explain the key differences and similarities between these two types, focusing on bipolar 1 vs 2.
Key Takeaways
Bipolar disorder is classified into two main types: Bipolar 1, characterized by severe manic episodes, and Bipolar 2, which includes hypomanic episodes and more frequent depressive episodes.
Diagnosis of bipolar disorder involves a comprehensive mental health evaluation, focusing on the severity and duration of manic and depressive episodes, with Bipolar 1 generally considered more severe.
Effective management of bipolar disorder typically requires a combination of medication, therapy, and lifestyle changes, with an emphasis on self-care and support systems to stabilize mood and reduce episode frequency.
Overview of Bipolar Disorder Types
Bipolar disorder is marked by pronounced fluctuations in mood, encompassing periods of mania or hypomania as well as episodes of depression. The condition manifests in two primary forms: Bipolar 1 and Bipolar 2, each impacting just above 1% of the population, while cyclothymic disorder is also acknowledged within the spectrum of mood disorders.
Within the United States, approximately 2.8% of adults have received a bipolar disorder diagnosis, highlighting its significance on a societal level. Typically, individuals with Bipolar 1 experience more intense disruptions to their daily lives compared to those living with Bipolar 2.
Understanding Bipolar 1
Bipolar 1 represents the most extreme variation of bipolar disorder, characterized by intense mood fluctuations. Individuals afflicted with this condition experience profound symptoms that encompass complete manic and depressive phases. The severity of manic episodes may necessitate hospital admission to mitigate hazardous actions or manage psychosis.
For a manic episode to qualify under Bipolar 1 criteria, it should persist for no less than one week or be severe enough to warrant inpatient care, whereas depressive periods typically extend over a minimum of two weeks. It’s frequent for people with bipolar during at least one such episode to make impulsive decisions involving activities like lavish spending.
Understanding Bipolar 2
Bipolar II is characterized by repeated instances of depressive episodes interspersed with at least one hypomanic episode, which is less severe than a full-blown manic episode. Instead of experiencing the extremes of mania, individuals with bipolar ii typically undergo periods of hypomania marked by uplifted spirits, heightened energy levels, and enhanced creativity—though these symptoms are not as acute as those found in manic episodes.
During a hypomanic episode, persons often exhibit elevated levels of energy and impulsiveness that can precipitate hazardous actions or create tension within interpersonal relationships. Hypomanic episodes can occur in many people who have bipolar disorder.
Key Differences Between Bipolar 1 and Bipolar 2
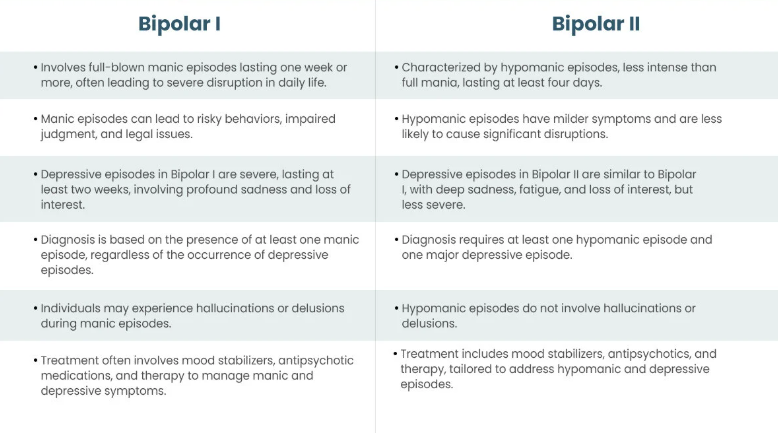
Bipolar 1 is characterized by the presence of manic episodes, in contrast to Bipolar 2, which encompasses hypomania and depressive episodes. The major distinguishing factor that classifies Bipolar 1 as more severe than Bipolar 2 lies in the severity of its manic episodes. The diagnosis of different types of bipolar disorder hinges on evaluating how long and how intense these manias, hypomanias or depressions are.
To summarize, while both conditions fall under the umbrella of bipolar disorder, it’s the intensity of manic symptoms that sets them apart: Bipolar 1 is acknowledged for its heightened level of mania compared to the milder manifestation found within Bipolar 2.
Severity of Episodes
Manic episodes in Bipolar 1 are more severe. Those with Bipolar 2 experience less intense hypomanic episodes. Hypomanic symptoms in Bipolar 2 are typically milder than those in Bipolar 1.
Mania leads to more noticeable issues, while hypomania is a milder form of the condition and has less severe symptoms.
Duration of Episodes
In Bipolar 1, manic episodes typically persist for a minimum of seven days, whereas hypomanic episodes in Bipolar 2 can vary in length but often span from several days up to one week.
Symptoms of Bipolar 1 and Bipolar 2
Bipolar disorder includes three types of episodes: mania, hypomania, and depression. The main difference is the severity of manic episodes, which are more intense in Bipolar 1. Bipolar 1 features more intense mania, while Bipolar 2 includes milder hypomanic episodes.
Common symptoms of Bipolar 1 include:
Grandiosity
Impulsivity
Irritability
Decreased need for sleep
Other symptoms
Manic episodes may cause severe issues at work, school, and social interactions, and can involve a manic episode with psychosis.
Manic Episodes in Bipolar 1
Core symptoms of Bipolar 1 manic episodes include elevated mood, high energy, irritability, impulsiveness, and risky behaviors. Manic episodes may also involve increased talkativeness, distractibility, and risky activities.
Severe mania can lead to psychosis, delusions, and hallucinations.
Hypomanic Episodes in Bipolar 2
Hypomanic episodes in Bipolar 2 can boost creativity and productivity, but are less severe than mania. Hypomanic behaviors often deviate from the individual’s usual state. Hypomanic symptoms last at least four days and are milder than manic symptoms.
Hypomanic episodes are less extreme, usually lack psychosis, and may be hard to recognize. During hypomania, individuals may make risky decisions and act hastily.
Depressive Episodes in Both Types
Individuals with bipolar disorder often endure a range of depressive symptoms, such as profound sadness, diminished interest in activities, sensations of insignificance, and alterations in eating and sleeping patterns. Typically, those suffering from this condition experience these signs of depression for a duration extending no less than two weeks.
In contrast to Bipolar 1 sufferers who might have fewer depressive periods, individuals diagnosed with Bipolar 2 frequently encounter more persistent forms of depression that prevail over extended timeframes. This can lead to an initial misdiagnosis for many people with Bipolar 2 because they tend to show signs of depression before any other symptoms.
Diagnosing Bipolar Disorders
The process of diagnosing bipolar disorder begins with an assessment of mental health carried out by healthcare professionals. This evaluation, frequently drawing upon research from jama psychiatry, is performed by a psychiatrist or licensed psychologist and includes a detailed review of the patient’s medical history and symptoms to ensure an accurate diagnosis.
To ascertain the specific variety of bipolar disorder, one must consult either a psychiatrist or a qualified mental health professional. For precise identification of Bipolar 2 in particular, an exhaustive examination conducted by such a mental health expert is crucial.
Diagnostic Criteria
The guidelines for identifying bipolar disorders have been established by the American Psychiatric Association. For a Bipolar 2 diagnosis, an individual must experience multiple depressive episodes and at least one hypomanic episode. Criteria distinguish between Bipolar 1 and Bipolar 2 diagnoses, with the former including severe manic episodes that may necessitate hospitalization.
Diagnosing individuals with Bipolar 2 can be challenging because they typically seek treatment when experiencing depressive episodes rather than during hypomanic states. To accurately diagnose any of the bipolar disorders, healthcare providers assess instances of manic, hypomanic, and depressive symptoms. It is also essential to exclude other possible causes such as substance abuse before confirming a diagnosis of Bipolar 1.
To eliminate alternative medical issues that could present similar signs to those of bipolar disorder, blood tests are conducted. Professionals evaluate the patient’s medical background along with their specific experiences pertaining to mania and depression in order to make an accurate assessment.
Mental Health Evaluation
Assessment of mental health conditions, including bipolar disorder, entails examining an individual’s psychological wellbeing and the severity of their symptoms. The process for diagnosing this specific mental health condition can involve a review of the person’s medical history, a detailed evaluation of their symptoms, and in some cases, performing blood tests to rule out other issues.
When significant symptoms indicative of either Bipolar I or II are present, it is important that the individual be referred to a specialist for evaluation and management.
Treatment Options for Bipolar 1 and Bipolar 2
Treating bipolar disorder usually involves combining therapy and medication. Medication and therapy are standard treatments for bipolar disorder. Significant lifestyle changes are crucial in treatment. Medication needs may vary, with Bipolar 1 often requiring higher doses than Bipolar 2. A psychiatrist helps find the right medication combination and monitors symptoms.
Active participation in treatment helps individuals effectively manage their symptoms. Difficulty adhering to treatment programs can affect bipolar disorder management. Identifying personal triggers and stressors is vital in managing bipolar disorders.
Depressive episodes can severely impair daily functioning, which can significantly impact the need for effective management during a major depressive episode.
Medication Management
Medications to manage bipolar disorder include mood stabilizers and antipsychotics. Mood stabilizers control manic or hypomanic episodes. Antipsychotics manage both manic and depressive symptoms. Doctors often start with a low dosage to gauge response.
Medications stabilize mood in bipolar disorder.
Talk Therapy and Support
Talk therapy is crucial in a bipolar disorder treatment plan. Cognitive behavioral therapy effectively treats bipolar disorder. Family-focused therapy is also valuable. Talk therapy helps patients identify triggers and establish coping strategies. A reliable support network enhances emotional well-being and aids in managing symptoms.
Psychoeducation improves treatment adherence by educating patients. Interpersonal and social rhythm therapy stabilizes daily routines, improving mood stability.
Self-Care and Lifestyle Changes
Implementing lifestyle adjustments plays a significant role in the effective control of bipolar disorders. Establishing a regular daily routine aids in mood stabilization and diminishes the occurrence of episodes. Engaging regularly in physical exercise is an essential element of self-care when dealing with bipolar disorder. Maintaining a steady sleep pattern is critical for preserving stable moods and promoting general mental health.
Participation in activities that enhance well-being is fundamental to symptom management for individuals with bipolar disorders. While hypomanic episodes can heighten productivity and creativity, they are not as severe as manic episodes. Emphasizing self-care practices along with making these lifestyle modifications has a positive influence on the handling of bipolar disorder symptoms.
Coping Strategies for Living with Bipolar Disorder
It is essential to maintain continuous treatment for the effective management of symptoms associated with bipolar disorder. Having a regular daily schedule can aid in controlling these symptoms. Activities that help reduce stress are vital for managing bipolar disorders effectively.
Creating a strong support network, handling stress and potential triggers appropriately, as well as focusing on self-care are fundamental strategies to cope with bipolar disorder.
Building a Support System
Relatives can play a crucial role by offering vital emotional support and assisting in keeping track of bipolar disorder symptoms. Participation in peer support groups for those with the condition bolsters a sense of community and empathy, while these groups offer camaraderie that mitigates feelings of solitude, making them critical for providing emotional backing and motivation.
For individuals coping with bipolar disorder, constructing a robust network of support is imperative as it delivers consistent emotional balance and positive reinforcement.
Managing Stress and Triggers
Managing coexisting related disorders and other mental health conditions is critical since they can intensify the symptoms of bipolar disorder. Initiating treatment for these health conditions early on is beneficial in curtailing the exacerbation of bipolar symptoms and mitigating stress.
For individuals with bipolar disorder, it’s imperative to stabilize mood by managing stress effectively and steering clear of triggers. Adopting a forward-thinking strategy for recognizing triggers and controlling stress plays an essential role in preserving mental health and overall well-being.
Prioritizing Self-Care
It’s essential for those managing bipolar disorder to emphasize self-care practices as a cornerstone of sustaining their mental health and well-being. Engaging in consistent routines that include:
frequent physical activity
nutritious eating habits
adequate rest
techniques for mindfulness
Fundamental components that can contribute to the stabilization of mood.
Fostering self-care is critical, as it can bolster emotional balance and fortify resilience, which equips individuals with better capabilities to navigate through the ups and downs associated with mood shifts. Making self-care a top priority is imperative.
When to Seek Emergency Help
Thoughts of suicide or self-harm indicate a need for immediate medical attention. Suicidal ideation can occur during bouts of depression and episodes of mania in individuals with bipolar disorder. If someone is having suicidal thoughts, dial 988 for crisis support.
In cases where someone is in immediate danger, call 911.
Summary
Grasping the fundamental distinctions between Bipolar 1 and Bipolar 2 is critical for proper identification and management. The former is defined by intense manic episodes, as opposed to the latter which features less severe hypomanic episodes coupled with repeated depressive instances. An exact diagnosis followed by detailed treatment strategies and steadfast support networks are pivotal in controlling symptoms and enhancing life quality. Individuals suffering from bipolar disorder can maintain satisfying lives through dedicated self-care, effective stress regulation, and cultivating a solid network of support.
Frequently Asked Questions
What are the main differences between Bipolar 1 and Bipolar 2?
The main difference between Bipolar 1 and Bipolar 2 lies in the severity of manic episodes; Bipolar 1 features severe manic episodes that may necessitate hospitalization, whereas Bipolar 2 is characterized by hypomanic episodes coupled with more persistent depressive episodes.
How long do manic and hypomanic episodes last?
Manic episodes in Bipolar 1 typically last at least seven days, while hypomanic episodes in Bipolar 2 last from a few days to a week.
Understanding these durations can be crucial in managing and identifying the condition effectively.
What are common symptoms of depressive episodes in bipolar disorder?
Common symptoms of depressive episodes in bipolar disorder include overwhelming sadness, loss of interest in previously enjoyed activities, feelings of worthlessness, and significant changes in appetite and sleep patterns.
Recognizing these symptoms is crucial for effective management of the disorder.
What are some effective treatment options for bipolar disorder?
An effective approach to treating bipolar disorder combines medication, such as mood stabilizers and antipsychotics, with talk therapy methods like cognitive behavioral therapy and family-focused therapy.
This multifaceted strategy can significantly enhance management of the condition.
When should someone with bipolar disorder seek emergency help?
Individuals with bipolar disorder should seek emergency help immediately if they experience thoughts of suicide or self-harm.
It is crucial to contact crisis support at 988 or call 911 in dangerous situations.
Author

Board-Certified Psychiatric Mental Health Nurse Practitioner with undergraduate degrees in Psychology and Philosophy (Summa Cum Laude) from Plymouth State University, and MSN degrees from Rivier and Herzing Universities. Specializing in PTSD, mood, anxiety, and personality disorders, with expertise in psychodynamic therapy, psychopharmacology, and addiction treatment. I emphasize medication as an adjunct to psychotherapy and lifestyle changes.